| Identification | Back Directory | [Name]
CETUXIMAB | [CAS]
205923-56-4 | [Synonyms]
IMC 225
CETUXIMAB
Hsdb 7454
EGFR antibody
Unii-pqx0D8J21j
CetuxiMab(C225)
CETUXIMAB USP/EP/BP
Cetuximab (anti-EGFR)
Cetuximab - Buffer solution
Immunoglobulin G1, anti-(human epidermal growth factor receptor) (human-mouse monoclonal C225 gamma1-chain), disulfide with human-mouse monoclonal C225 kappa-chain, dimer | [Molecular Formula]
C6484H10042N1732O2023S36 | [MDL Number]
MFCD06407972 | [MOL File]
205923-56-4.mol | [Molecular Weight]
2756.23 |
| Hazard Information | Back Directory | [Description]
Cetuximab, a human/mouse chimeric monoclonal antibody that blocks the EGFR,
was launched for use in combination with irinotecan in the treatment of patients with colorectal cancer who no longer respond to standard chemotherapy
treatment with irinotecan. Cetuximab is obtained by chimerization of M225, a
murine anti-EGFR antibody; specifically heavy and light chains of the murine
antibody are cloned and adapted for expression with constant regions of the human
kappa light chain and human gamma1 heavy chain. It is produced by mammalian
(suspension) cells in serum-free medium, purified by protein A affinity chromatography,
ion-exchange chromatography, and gel filtration. Cetuximab binds specifically
to EGFR on both normal and tumor cells. Overexpression of the human EGFR is
detected in many cancers, including those of the colon and rectum. The binding of
cetuximab to EGFR prevents growth factors from binding to the receptor, thereby
inhibiting cell growth and inducing apoptosis. The therapeutic regimen of cetuximab
consists of an initial loading dose of 400 mg/m2 administered as a 120-min IV
infusion, followed by weekly maintenance dose of 250 mg/m2 infused over 60 min.
The steady-state plasma concentrations of cetuximab are reached by the third weekly
infusion and the mean elimination half-life is 114 h. Cetuximab is eliminated by
binding to EGFRs in various tissues, followed by internalization of the antibody-
EGFR complex. Systemic clearance of the antibody is saturated at higher doses, and
this appears to correlate with saturation of EGFR binding. In a multicenter clinical
trial in more than 300 patients with advanced metastatic colorectal cancer,
combination therapy with cetuximab and irinotecan produced response in more
than half of the patients, shrinking tumors in 23% and stopping tumor growth in an
additional 33% of the patients. The most common adverse reactions associated with
cetuximab were acneform rash, asthenia/malaise, fever, nausea, abdominal pain,
constipation and vomiting. Serious adverse events such as infusion reaction, fever,
sepsis, kidney failure, dehydration and diarrhea were experienced by <10% of the
patients. | [Originator]
ImClone (US) | [Uses]
Treatment of EGF receptor-expressing cancers
(monoclonal antibod. | [Brand name]
Erbitux | [Mechanism of action]
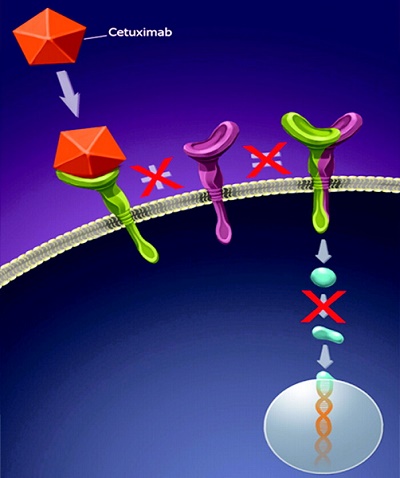
Cetuximab, a monoclonal antibody, binds to the extracellular domain of the EGFR, which is overexpressed in many human cancers, including head, neck, and colorectal types. This process prevents the EGFR from binding with its endogenous ligand, blocking the receptor-dependent transduction pathway and providing many antitumor effects involving cell-cycle arrest, induction of apoptosis, inhibition of angiogenesis, inhibition of metastasis, internalization, and downregulation of the EGFR, and enhancement of the sensitivity to radiochemotherapy[1].
| [Clinical Use]
Monoclonal antibody:
Treatment of EGFR-expressing metastatic colorectal
cancer in combination with irinotecan after failure of
irinotecan-including cytotoxic therapy
Treatment of head and neck cancer | [Toxicology]
The majority of skin toxicities were mild to moderate, symptomatic treatments were effective in controlling them. The skin discomfort caused by cetuximab can affect the quality of life temporarily; with long term treatment, severity of skin toxicity may decrease.
| [Drug interactions]
Potentially hazardous interactions with other drugs
Avoid with live vaccines. | [Metabolism]
Several pathways have been described that may contribute
to the metabolism of antibodies. All of these pathways
involve the biodegradation of the antibody to smaller
molecules, i.e. small peptides or amino acids. | [References]
[1] W Bou-Assaly, S Mukherji. “Cetuximab (erbitux).” American Journal of Neuroradiology 31 4 (2010): 626–7.
|
|
|